Insulin Resistance: Causes, Effects, and Management Strategies
Insulin resistance, a condition where cells fail to respond to insulin properly, is a significant health concern worldwide. Insulin resistance is the main precursor to a host of chronic medical disorders, including dementia, hypertension, obesity, cardiovascular disease, erectile dysfunction, type 2 diabetes, cancer, chronic kidney disease, PCOS, fatty liver disease. Understanding its diverse causes and implementing effective management strategies is crucial for mitigating its detrimental effects on health. In this comprehensive guide, we delve into the various contributors to insulin resistance and explore evidence-based treatment approaches to address this complex metabolic phenomenon.
- Genetic Predisposition: Genetic variations in insulin signaling pathways, such as the IRS1 and IRS2 genes, can predispose individuals to insulin resistance. While genetic factors cannot be altered, lifestyle modifications and targeted therapies can help mitigate their impact on insulin sensitivity.
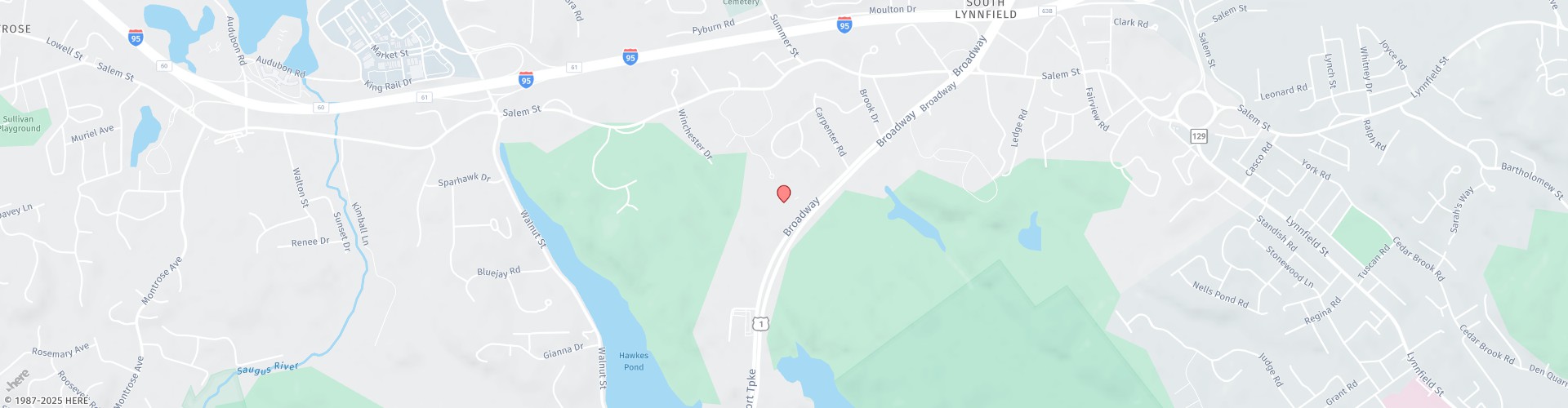
- Obesity: Excess adipose tissue, particularly visceral abdominal fat, releases inflammatory molecules that interfere with insulin signaling, promoting insulin resistance. Weight management through calorie control, physical activity, and dietary changes is crucial for improving insulin sensitivity in individuals with obesity. Drugs such as GLP-1 agonists (semaglutide and tirzepatide) can help treat obesity when combined with a very low carbohydrate/low fat diet. Here is information on our weight loss program, which is very effective in treating obesity and insulin resistance.
- Sedentary Lifestyle: Lack of physical activity reduces glucose uptake by muscles, contributing to insulin resistance. Regular exercise, including aerobic activities, resistance training, and high-intensity interval training, enhances insulin sensitivity and promotes glucose utilization by muscles.
- Poor Diet: High intake of refined carbohydrates, saturated fats, and sugary foods can induce insulin resistance by promoting inflammation and lipid accumulation in tissues. Adopting a balanced diet rich in phytonutrients and antioxidants, low-glycemic carbohydrates, vegetables, lean proteins, and healthy fats can help improve insulin sensitivity and metabolic health.
- Chronic Stress: Prolonged stress activates the hypothalamic-pituitary-adrenal (HPA) axis and sympathetic nervous system, leading to increased cortisol and catecholamine levels, which contribute to insulin resistance. Stress-reduction techniques such as mindfulness meditation, yoga, and deep breathing exercises can help lower cortisol levels and improve insulin sensitivity.
- Sleep Deprivation: Inadequate sleep disrupts hormonal balance, increasing cortisol levels and reducing insulin sensitivity. Prioritizing quality sleep through lifestyle adjustments and creating a conducive sleep environment promotes hormonal balance and metabolic health.
- Inflammation: Chronic low-grade inflammation, often associated with conditions like obesity and metabolic syndrome, can impair insulin signaling pathways. Consuming anti-inflammatory foods rich in omega-3 fatty acids, antioxidants, and phytonutrients can help combat inflammation and improve insulin sensitivity.
- Hormonal Imbalance: Conditions such as polycystic ovary syndrome (PCOS) and Cushing’s syndrome, characterized by hormonal dysregulation, can lead to insulin resistance. Management of underlying hormonal imbalances, along with lifestyle modifications and targeted therapies, is essential for improving insulin sensitivity in these individuals.
- Environmental Toxins: Exposure to environmental pollutants such as persistent organic pollutants (POPs), heavy metals, and endocrine-disrupting chemicals (EDCs) has been linked to insulin resistance. These chemicals are found in plastics, pesticides, herbicides, chemicals, food additives. Minimizing exposure to toxins through lifestyle adjustments is crucial for preserving metabolic health.
- Gut Microbiota Dysbiosis: Imbalance in the composition of gut microbiota can contribute to insulin resistance through mechanisms involving inflammation, altered gut barrier function, and production of metabolites that affect insulin sensitivity. Restoring gut microbial balance through dietary changes and targeted interventions may alleviate insulin resistance.
- Medications: Certain medications, including corticosteroids, antipsychotics, beta-blockers, and protease inhibitors, have been associated with insulin resistance as a side effect. Healthcare providers may explore alternative medications or adjunct therapies to mitigate insulin resistance in individuals experiencing medication-induced metabolic effects.
- Sleep Apnea: Obstructive sleep apnea disrupts sleep patterns causes release of the stress hormone cortisol and promotes oxidative stress, culminating in insulin resistance. Treatment strategies such as continuous positive airway pressure (CPAP) therapy, weight loss, and lifestyle modifications aim to improve sleep quality and alleviate insulin resistance.
- Chronic Infections: Persistent viral or bacterial infections contribute to insulin resistance through chronic inflammation and immune dysregulation. Targeting the underlying infection with appropriate medical interventions alongside lifestyle modifications may ameliorate insulin resistance.
- Excessive Fructose Consumption: High intake of fructose, prevalent in processed foods and sugary beverages, fosters lipid accumulation in the liver and impairs insulin signaling. Dietary modifications emphasizing whole foods and reduced sugar intake are pivotal in combating fructose-induced insulin resistance.
- Alcohol Overconsumption: Alcoholic beverages contain empty calories, contributing to obesity and increased visceral fat; alcohol causes liver damage and increases risk of fatty liver and is directly inflammatory, increasing oxidative stress in the body, which increases IR; alcohol adversely affects hormone levels including growth hormone, cortisol, and glucagon, alcohol is a cause of gut damage (leaky gut) which is inflammatory, and is associated with dysbiosis of the gut microbiota, and finally, alcoholism is associated with nutritional deficiencies such as thiamine and magnesium, that can aggravate insulin resistance.
Treatment Strategies for Insulin Resistance: Addressing the multifactorial nature of insulin resistance requires a comprehensive approach involving lifestyle modifications, dietary interventions, stress management, and, in some cases, pharmacotherapy. Personalized interventions tailored to individual needs and underlying factors are essential for optimizing metabolic health and reducing the risk of developing type 2 diabetes and other metabolic complications.